When parents who are at risk of having a child with an inherited genetic disease explore the option of having their embryos tested via preimplantation genetic testing (PGT), they are often surprised to learn that they have to start by creating those embryos with in vitro fertilization (IVF). Thus, it’s common for intended parents to ask: “What is IVF?”
What Is IVF?
IVF is a multi-step procedure used to treat fertility or genetic problems. The term “in vitro” refers to procedures that are done outside of a living body and in an artificial environment. In the case of IVF, a woman’s eggs are fertilized by sperm in a laboratory instead of inside a Fallopian tube. IVF is the most advanced and effective fertility treatment available today.
What Are the Steps for IVF?
Your fertility specialist may do a series of tests to determine if you and your partner are good candidates for IVF, such as semen analysis, hormone testing and infectious disease screening. Once approved for the procedure, IVF typically involves the following steps:
Step 1: Medication To Stimulate Growth of Multiple Eggs
An average menstrual cycle lasts about 28 days, and involves the release and maturation of one egg cell from the ovary and the preparation of the uterus for pregnancy. This process is triggered by the natural release of hormones, such as estrogen.
In an IVF cycle, woman are given injectable medications to self-administer in order to stimulate the development of multiple eggs within the ovary or both ovaries. These medications are taken for about eight to 14 days. The purpose of stimulating multiple eggs at once is to increase the chance of creating a healthy embryo. Medications are also taken to prevent the body from releasing developing eggs too soon and to prepare the lining of the uterus for implantation of the embryo.
Step 2: Retrieval of Eggs From the Ovary or Ovaries
Prior to retrieving the eggs, the doctor will perform a transvaginal ultrasound to examine the ovaries and perform a blood test on the woman to see how her body is responding to the medication. Women are given a “trigger shot” and return to the clinic about 36 hours later.
General anesthesia is administered for any pain or discomfort. Eggs are retrieved with a transvaginal needle by the fertility specialist using an ultrasound probe to guide them. The process takes about 20 to 30 minutes. All of the collected eggs are placed within a cultured medium and incubated.
Women going through the IVF process on average have about 10-15 eggs harvested per cycle. However, predicting the number of eggs per patient is very difficult. Some women may produce over 30 eggs, while others may not produce any. Factors include age and how well they respond to the hormone medications. Retrieval of more eggs maximizes the chances of having more babies born per retrieval and minimizes the number of IVF cycles necessary to build a family.
Step 3: Fertilization
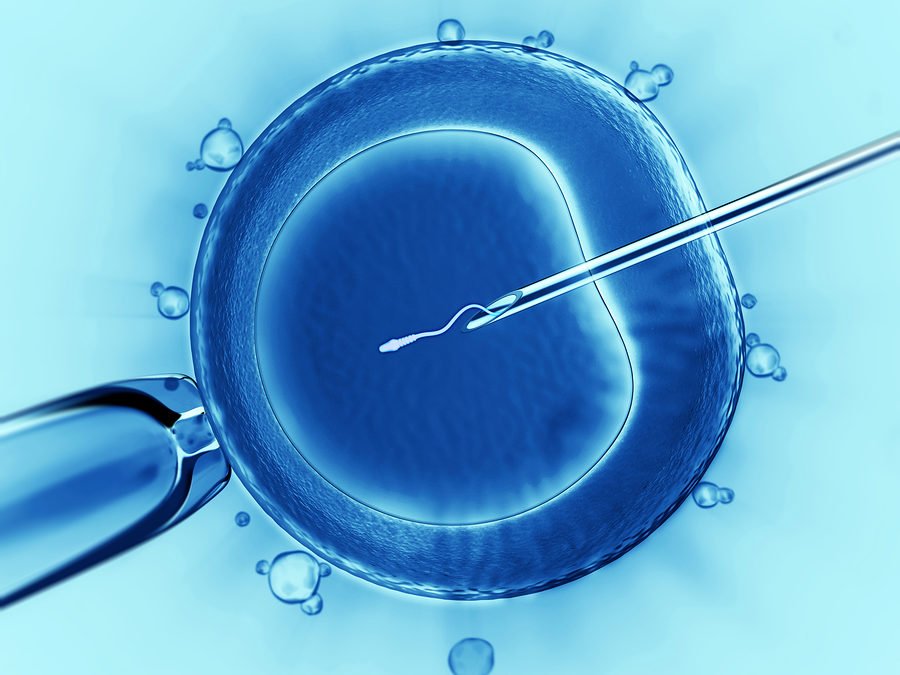
An egg cell must be fertilized with a sperm cell in order for an embryo to be created. While conventional fertilization involves surrounding an egg with healthy sperm and allowing a sperm to penetrate the egg cell on its own, intracytoplasmic sperm injection (ICSI) involves the embryologist injecting a single sperm into the egg cell under the guidance of a microscope.
Step 4: Embryo Development With Genetic Screening/Testing
All the fertilized eggs are incubated to allow them to grow from a single-cell to a multiple-cell embryo. On day five post-fertilization, healthy embryos should have developed into a ball of cells called a blastocyst.
In a process called a trophectoderm biopsy, about five to 10 cells are removed from the blastocyst in an area that will eventually become the placenta. These cells are sent to the laboratory for any elected genetic screening or testing, which includes PGT if the embryo is at risk of inheriting a specific genetic condition based on a known mutation or mutations that one or both parents carry.
Because the IVF and PGT process may take several weeks, the embryos are kept at the fertility clinic and cryopreserved using a freezing process that allows for the embryos to later be thawed and continue to develop if selected for uterine transfer.
Step 5: Embryo Transfer
After results are returned from the laboratory, the embryologist will inform the intended parents about the general quality and genetic health of each embryo and, if desired, the sex. The fertility specialist will often suggest transferring a single healthy embryo to increase the chances of a healthy pregnancy.
After the intended parents select an embryo, the transfer process is quick and painless. The doctor uses a catheter and an abdominal ultrasound to guide the embryo, where it is transferred onto the uterine wall. After the embryo is transferred, women are given injectable or vaginal progesterone to support the healthy lining of the uterus and aid with embryo implantation.
Patients have to wait two weeks until pregnancy is verified with a pregnancy test, which is often described as the hardest part of the process. If the pregnancy is successful, the patient’s OB-GYN will continue care of the pregnancy and recommend prenatal screening or testing to verify all preimplantation genetic testing results. If the pregnancy is not successful, couples may choose to try another embryo transfer with one of the other healthy embryos or start another IVF cycle to try again.
While there are many different steps to the IVF and PGT process, the team of doctors, nurses, genetic counselors, care coordinators and technicians are there to help with any questions that patients have on the road to building their family.

Leslie is a board-certified clinical genetic counselor and former Program Manager for the preimplantation genetic testing (PGT) program of the ORM Genomics team and former Project Manager for SharingHealthyGenes.com. She completed her Bachelor’s degree at DePauw University and her Master’s degree in Genetic Counseling at the University of Texas Graduate School of Biomedical Sciences at Houston. Since graduating in 2000, she has worked as a clinical genetic counselor in several specialties including prenatal, pediatric and cancer genetics and has been very involved with the National Society of Genetic Counselors.