Colorectal cancer is fairly common for both men and women in the United States. The lifetime risk for developing colorectal cancer is 1 in 22 for men and just slightly lower for women (1 in 24). There are many factors that can increase the risk of developing colorectal cancer. One of those is a hereditary cancer syndrome called familial adenomatous polyposis (FAP). FAP accounts for about 1% of all colorectal cancers. Almost everyone with FAP will develop cancer by age 40. Preimplantation genetic testing (PGT) offers an option for individuals with FAP to avoid passing on this cancer risk to their children.
What is FAP?
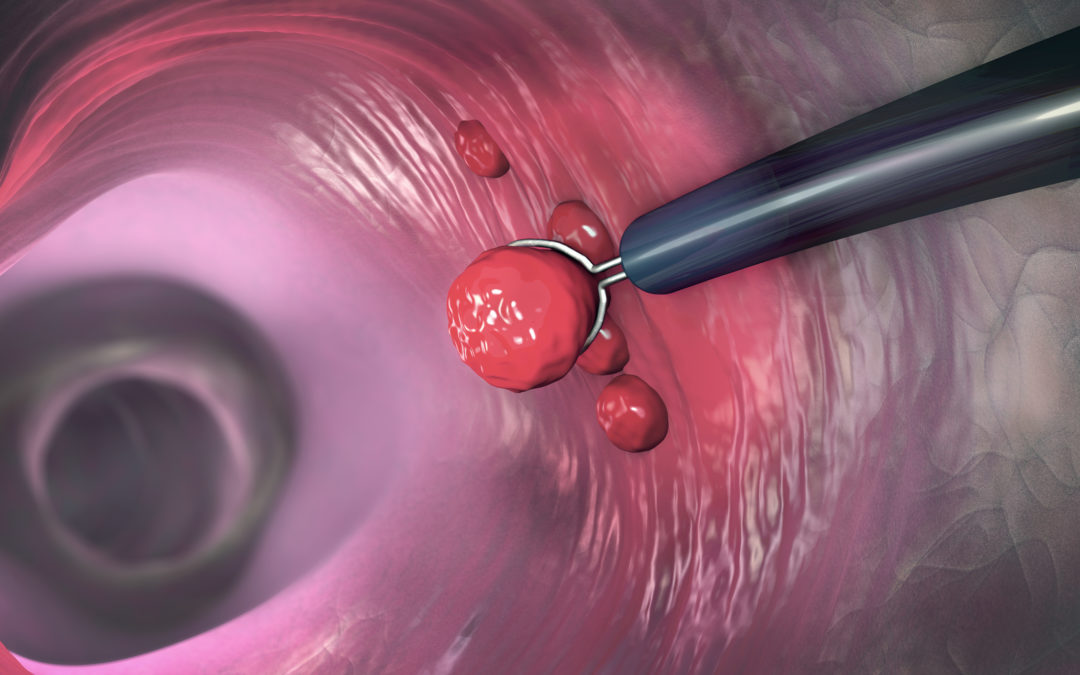
FAP is a hereditary cancer syndrome that significantly increases the risk for colorectal cancer as well as cancers in other organs including the stomach, small intestine, and pancreas. Often, the precursor to cancer development is the presence of polyps. Colon polyps are small groupings of cells that form on the inside of the colon. Most polyps are harmless, but over time, they can become malignant (cancerous). People with FAP begin to develop polyps in their mid-teens and can progress to having hundreds of polyps over time. Without treatment, the risk of colorectal cancer is almost 100% due to the sheer number of polyps and the likelihood that one or more will eventually turn malignant.
There are several subtypes of FAP. Individuals with Attenuated FAP (AFAP) have significantly fewer polyps (20-100) and may develop cancer later in life.
How is FAP inherited?
FAP is an autosomal dominant disorder caused by a mutation in the APC gene. Individuals have two copies of each gene, one that they inherit from their mother and the other from their father. In FAP, it only takes a mutation in one copy of gene to cause the disease. Therefore, a parent with FAP has a 50% chance of passing the APC mutation down to their child.
The majority (70-80%) of FAP cases are inherited. However, in the remaining cases there is no family history of the condition, and it is expected that the condition arose from a de novo, or new mutation in that individual. This is an important consideration for PGT. A parent with a de novo mutation would have a 50% chance of passing that mutation on to a future pregnancy whereas de novo cases of FAP in a previous child or family member would not be expected to increase the risk.
How is FAP treated?
The American Society of Clinical Oncology (ASCO) recommends that individuals with a family history of FAP begin colorectal cancer screening with yearly colonoscopy in their early teens. Once polyps develop, however, there is little that can be done to prevent cancer from growing except removal of part or all of the colon. This procedure, called a colectomy, is recommended when the number of polyps prevents effective screening with colonoscopy or when cancer is suspected.
Is preimplantation genetic testing (PGT) available for FAP?
Yes. PGT (also referred to as preimplantation genetic diagnosis or PGD) is available for individuals with a personal history of FAP. Historically, PGT for FAP has been somewhat controversial given that cancer does not typically develop until the adult years. However, given that symptoms begin in the teenage years, screening via colonoscopy is highly invasive, and undergoing a colectomy to prevent cancer results in its own lifelong challenges, some high risk families would prefer to have alternate options for conception like PGT. A recent study showed that at least a third of individuals with FAP would consider PGT for themselves. Professional societies support the use of PGT in cases like FAP where the condition is serious and the available intervention is particularly burdensome. Because of the complexity of performing PGT for genetic disease, working with fertility clinics who are experienced with this technology and invest in genetic counselors to help patients through this journey is essential.
For more information on peer support for FAP, check out Hereditary Colon Cancer Takes Guts. To learn more about research and advocacy for colorectal cancer, go to Fight Colorectal Cancer.

Jessica Greenwood is an independent consultant to Sharing Health Genes. As a licensed genetic counselor and digital health consultant, she works with health-related organizations looking to deliver memorable messages of health in the digital space. Mrs. Greenwood started her career in a clinical role, working for eight years as a preconception and prenatal genetic counselor before transitioning to industry. Mrs. Greenwood completed a year-long certificate program in Digital Health Communication at Tufts University that spearheaded her work in digital health. She now consults with health-related organizations, assisting with the creation and execution of a digital strategy including the development of health literate patient-centered educational materials. Mrs. Greenwood earned a Bachelor of Science degree from North Carolina State University with a minor in Genetics and a Master of Science in Genetic Counseling from the University of North Carolina at Greensboro.