Autosomal dominant is a pattern of inheritance. Genetic diseases are caused by gene changes, also called mutations or pathogenic variants that cause the gene not to work properly. We inherit two copies of each gene from our parents; one from our mothers and the other from our fathers. Sometimes a person must inherit two mutations (i.e. one from each parent) in order to have an increased risk to develop the disease, which is called autosomal recessive inheritance. For autosomal dominant diseases, however, a person must inherit just one mutated copy of the gene in order to have the genetic disease. In essence, the mutated copy “dominates” the non-mutated copy. Usually a person inherits the mutated copy from a parent who has the disease. In some cases, a new mutation can occur when an embryo is created making that person the first one affected with the condition in the family. Because the mutation is on a non-sex chromosome, it can affect men and women equally.
What are some examples of autosomal dominant diseases?
There are several different kinds of autosomal dominant diseases that can lead to intellectual disability and/or physical differences from birth. For example, achondroplasia is an autosomal dominant disorder that can be identified by ultrasound by observing that the long bones of the arms and legs are shorter than expected. The FGFR3 gene is important for normal skeletal development. People with achondroplasia have one copy of the FGFR3 gene that has a change, causing the short stature and other physical differences and health problems. About 20 percent of babies born with achondroplasia have inherited a pathogenic variant in the gene from a parent who also has achondroplasia. About 80 percent of the time, children are born to average sized parents and have a new mutation.
Other autosomal dominant diseases can be progressive throughout childhood and adulthood. Neurofibromatosis type 1 (NF1) is a disease that usually appears in early childhood, starting with the emergence of cafe-au-lait spots, which are darker, flat patches of skin. These patches grow in size and number as an individual gets older. Other symptoms such as non-cancerous tumors called neurofibromas can appear over the years.
What is the chance to develop the disease if you have an autosomal dominant mutation?
It depends on the disease. For example, all people with a disease-causing mutation in FGFR3 will have features of achondroplasia visible from birth. Autosomal dominant polycystic kidney disease (ADPKD) is a disease that affects all people who have a pathogenic variant in PKD1, but cysts within the kidneys usually don’t appear until childhood. Huntington’s disease is another disorder where there is a 100 percent chance of developing the disease, but some people with the mutation may develop the disease at an earlier age compared to others. Symptoms of Huntington disease usually develop between ages 30 and 50, but they can appear as early as age 2 or as late as 80. 
There are several disorders where a person who has a mutation that causes the autosomal dominant disease is at an increased risk for developing symptoms of the disease, but that risk is not 100 percent. These diseases include most hereditary cancer syndromes such as Lynch syndrome, and inherited cardiovascular disorders, such as long QT syndrome.
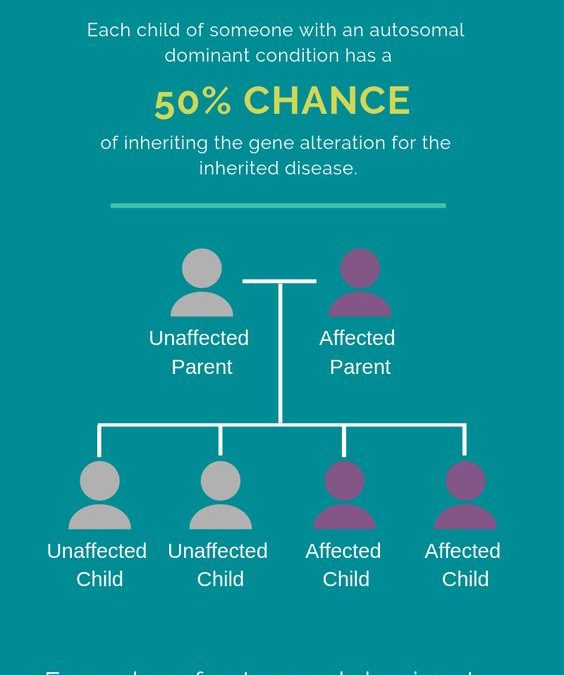
What is the chance a parent affected by an autosomal dominant disease can have an affected child?
Recall that each person has two copies of each of the ~20,000 genes in the human genome. A parent who has an autosomal dominant disorder has a pathogenic variant in one copy of their genes and a normal version in the other copy. There is a 50% chance that the parent can pass on the normal copy and a 50% chance that they pass on the copy with the pathogenic variant. Thus, there is a 50% chance that a child of a parent with an autosomal dominant disorder will also inherit the disease.
Can preimplantation genetic testing be done for autosomal dominant diseases?
Preimplantation genetic testing (PGT) is commonly offered to parents who have a known pathogenic variant for an autosomal dominant disease. While the exact number of IVF cycles using the technology is unknown, the list of diseases where PGT has been successful includes many autosomal dominant diseases, and it continues to grow. Many factors play a role in whether or not parents decide to pursue PGT. Meeting with a genetic counselor before you become pregnant is the best next step to explore your risk to have a child with an autosomal dominant disease and discuss the option of PGT.

Leslie is a board-certified clinical genetic counselor and former Program Manager for the preimplantation genetic testing (PGT) program of the ORM Genomics team and former Project Manager for SharingHealthyGenes.com. She completed her Bachelor’s degree at DePauw University and her Master’s degree in Genetic Counseling at the University of Texas Graduate School of Biomedical Sciences at Houston. Since graduating in 2000, she has worked as a clinical genetic counselor in several specialties including prenatal, pediatric and cancer genetics and has been very involved with the National Society of Genetic Counselors.